As a result of holiday gatherings, African officials warn of a resurgence of COVID-19 on the continent and urge increased testing to combat it.
The level of testing across the continent is considerably less than what health experts say is needed to effectively control the spread of the disease.
Africa makes up about 3.3% of the global total of confirmed virus cases, but this is believed to be just a fraction of the actual cases on the continent of 1.3 billion people.
When the pandemic began only two of Africa’s 54 countries had laboratories to test for the disease. Now virtually every one of the continent’s countries can carry out the tests. Together Africa’s countries have conducted at least 25 million COVID-19 tests, with a recent increase of 3%, according to the Africa Centers for Disease Control and Prevention.

Compared to the small amount of testing at the beginning of the pandemic, Africa CDC Director John Nkengasong has said the increased testing is “good progress and we continue to be hopeful of this.”
The distribution of the tests, however, is very uneven. Just 10 countries — South Africa, Morocco, Ethiopia, Egypt, Kenya, Ghana, Nigeria, Uganda, Rwanda and Cameroon — are carrying out more than 70% of the continent’s testing. To make the testing more widespread, 2.7 million additional tests have been procured by member states, the Africa CDC said some weeks ago.
Increased testing is needed to help Africa locate where cases are rising and where additional medical responses are needed. And, when they become available to Africa, where vaccines should go.
READ MORE: Another new variant of COVID-19 has emerged in Nigeria
Africa’s rural areas have even less testing than its cities, where most hospitals and clinics are located. More testing is needed in rural areas, said Nkengasong, especially as urban Africans travel to remote areas to unite with their families as the New Year approaches.
Rapid antigen tests would dramatically boost the ability to test in Africa’s remote, rural areas, according to the Africa CDC and WHO.
The rapid tests look for antigens, or proteins found on the surface of the virus. They are generally considered less accurate — though much faster — than PCR tests, which are higher-grade genetic tests. PCR tests require processing with specialty lab equipment and chemicals and it can take several days before patients get the results.
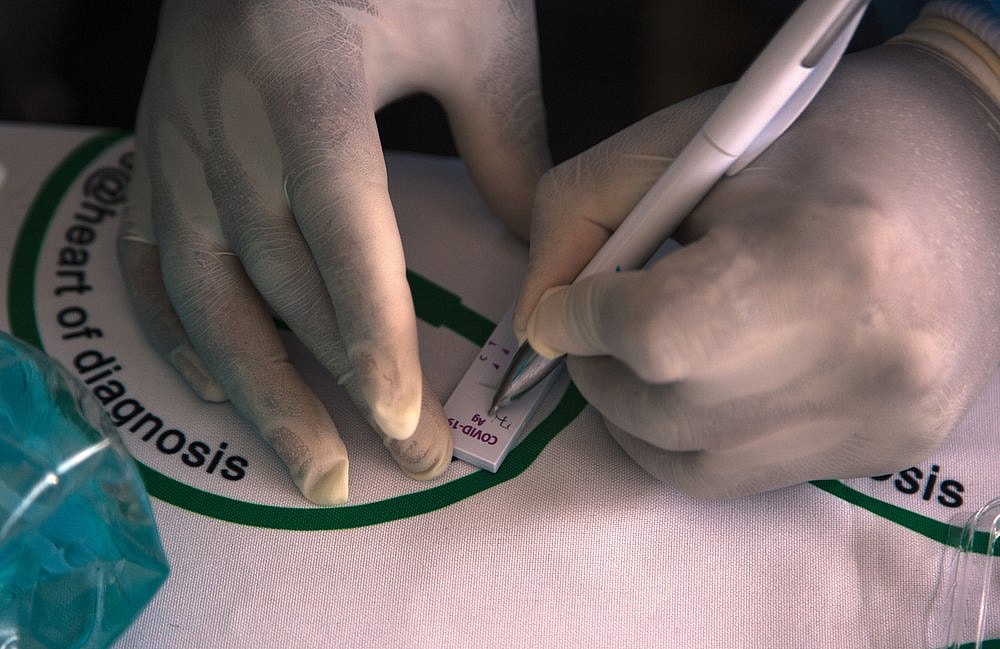
In contrast, the rapid antigen tests can provide results at the testing site in less than 30 minutes.
The World Health Organization and its partners announced in September that 120 million of the rapid tests would be made available to help Africa’s poor and middle-income countries test at levels closer to those of richer countries, which are deemed necessary to effectively fight the spread of COVID-19.
“Once we begin to use the antigen test more broadly, it will become a game-changer aspect of the way we do testing for the across the continent, especially in the remote areas and especially during this holiday period,” said Nkengasong.
Dr. Matshidiso Moeti, WHO’s regional director for Africa, has said that many cases remain unrecorded in Africa, because of the lack of testing, which has focused on travelers, patients and direct contacts. Few African countries have been able to do adequate community testing to find where the disease is concentrated and at what level.
Laboratory capacity for testing in African nations is lower than in most countries, according to WHO, calling testing volumes sub-optimal due to limited supplies of PCR test kits, which can be expensive.
“The global demand has put a strain on the supplies, with delays and some of the countries have inadequate infrastructure for setting up labs with molecular testing capacity for PCR diagnosis of COVID-19,” according to the WHO.
Prof. Pontiano Kaleebu, who heads an agency in charge of testing for the coronavirus in Uganda, said in many African countries people cannot afford the tests.
Testing fees in Uganda range from $65 to $100, and the service is not available in many remote areas.

“Sometimes people keep saying, ‘Where do I go? What do I do?’” he said, referring to patients who need to take a COVID-19 test but lack the money or don’t know of a nearby testing facility.
According to Ugandan government guidelines, hospitals are ordered to isolate patients who show COVID-19 symptoms on admission, but others on routine visits to health facilities aren’t necessarily tested and must pay out of pocket if they wish to be tested.
Officials standing guard at hospital entrances conduct temperature checks and desultorily take notes, but some visitors can pass through undetected when the guards are tired or have gone for a lunch break.
Uganda, which has tested over 736,000 samples for COVID-19, has reported nearly 34,000 cases and 248 deaths as of Dec. 30.
“If we had all the resources, we would test more,” Kaleebu said.
READ MORE: Doctor who discovered Ebola warns of more viruses after COVID-19
The World Health Organization recommends that countries should not be finding more than about 5% of all cases they test to be positive, suggesting that above that threshold they aren’t testing widely enough.
In Africa, the positivity ranges from 2.3% to more than 40%, according to Our World in Data, which compiles data from Johns Hopkins University. In Europe, however, the range is similar, from 5% to more than 30% in some countries.
However, when looking at the tests carried out per 1,000 people, African countries are on the low end ranging from 0 to the highest in Morocco at 119 tests per 1,000 people, according to the data.

In efforts to track the level of infections in communities, countries such as South Africa and Ghana are testing for the prevalence of COVID-19 in sewage water.
In South Africa, which has conducted more than 5.6 million tests, the Water Research Commission at wastewater treatment plants found COVID-19 fragments in sewage, mainly human feces, which corresponded with official numbers on the prevalence of the virus, especially in hotspot areas.
Water samples are drawn from water treatment facilities serving residential and commercial areas, but the research has been widened to include non-sewered areas in South Africa’s poor and overcrowded informal settlements.
“In South Africa, the number of COVID-19 patients are most likely underestimated, mainly due to the limitations regarding testing and also due to the likely large number of asymptomatic individuals,” said Jay Bhagwan, executive manager for water use and waste management of the Water Research Commission.
“If we can rapidly expand the wastewater surveillance program in South Africa, the sector will have a tool that provides valuable additional information about the spread of the virus as a complement to health surveillance.”
Have you subscribed to theGrio’s podcast “Dear Culture”? Download our newest episodes now!
TheGrio is now on Apple TV, Amazon Fire, and Roku. Download theGrio today!

