What do you know about PCOS?
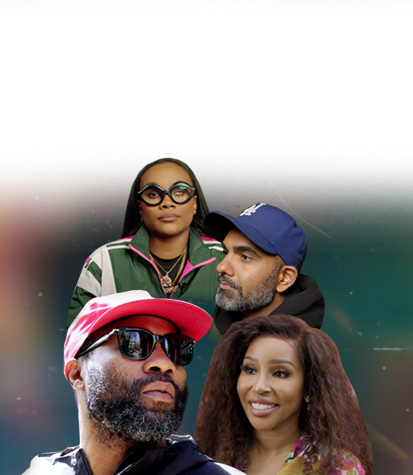
Keke Palmer’s pregnancy announcement was a spark of hope for those who understand the challenges of PCOS. An expert explains the condition that can impact reproductive health.
While hosting last weekend’s “Saturday Night Live,” actress Keke Palmer used her opening monologue to reveal she is expecting her first child. It was a reveal met with much joy from her fans and the general public, particularly those who suffer from polycystic ovary syndrome (PCOS), a condition that can have a major impact on a person’s reproductive health.
According to the CDC, 6 percent to 12 percent (roughly five million) of women are impacted by this disease. Palmer has openly discussed being one of them.

The disease can have far-reaching consequences for some patients but as we learned during a conversation with Dr. Chantel Cross, Johns Hopkins’ director of reproductive endocrinology and infertility fellowships, it’s not a completely hopeless situation for most. TheGrio sat down with Cross, who is also an assistant professor of gynecology and obstetrics, to discuss what the disease is and how it’s managed, and to shed light on what’s misunderstood about life with PCOS.
One thing she made clear: “PCOS is not birth control.”
theGrio: What exactly is Polycystic Ovary Syndrome?
Dr. Chantel Cross: Polycystic ovary syndrome is one of the most common hormone abnormalities that affect women. It is a syndrome that leads to irregular or inconsistent ovulation patterns, which patients experience as irregular periods. It is also associated with other symptoms, like acne or excessive hair growth on the face or other parts of the body, and can put them at risk for other medical problems like diabetes and other medical conditions.
TG: What are any known causes or risk factors associated with developing PCOS?
CC: PCOS is a very complex disease. We say that it’s polygenic, meaning there are multiple different genes that have been associated with the development of PCOS. But there are also many different causes that are not genetic. It’s not always the specific gene mutation and it affects many different organ systems, including your liver, your mood, [and] your heart. It’s a super complex condition so we don’t have one single positive thing that leads to it. We know it can run in families but the exact cause is unknown.
TG: How do you know if you have it?
CC: The most common thing that patients will come in with or complain of is that their periods are irregular or [in more severe cases] that they don’t have periods. Other patients or women will come in later on in life when they’re trying to become pregnant because they are having trouble getting pregnant.
But I’d say most people are diagnosed probably in their adolescence, shortly after they first start having their period, because that’s when most people will kind of start having the symptoms of skipped or irregular periods.
TG: How specifically does having PCOS impact a person’s ability to get pregnant?
CC: You can have different severities of PCOS. The easiest way to understand is the subgroup of patients who never ovulate. So they don’t get periods on their own at all. They’re obviously going to have a really hard time getting pregnant because they aren’t releasing an egg at all. That obviously is a big barrier to their fertility.
In other patients who may have irregular or inconsistent ovulation, [that] means they ovulate every two or three months. So [because an egg is still being released] there are opportunities for them to conceive. If they have no idea when [ovulation] is going to be, it’s really hard to operate that with their partner to try and conceive. There are also less opportunities for them to get pregnant if there are fewer ovulations a year, so it’s going to take them longer to get pregnant.
TG: Are there ways they can be helped along in the process?
CC: There are definitely ways to help someone who is trying to get pregnant to ovulate on a more consistent basis. We use something called “ovulation induction,” which is usually medication that we prescribe through your OBGYN or through a fertility center. Those medications can increase the likelihood of releasing an egg on a more monthly basis, and then we can help them time their intercourse or plan fertility treatments around that ovulation.
TG: How else can PCOS affect someone’s life?
CC: PCOS is associated with many other medical conditions. The fact that it’s called “polycystic ovarian syndrome” means that it’s going to affect multiple organ systems. It increases the likelihood of developing type-2 diabetes; it increases the likelihood of increased high blood pressure. High cholesterol, heart disease, depression, anxiety and uterine cancer are all other conditions patients with PCOS are more at risk for. They also have a higher likelihood of being overweight and more difficulty losing weight. There is also an increased risk for sleep apnea and increased risk for certain liver disorders.
TG: How can this condition and its potential consequences be managed?
CC: Seek evaluation with an OBGYN if you think you may have PCOS or if you have irregular periods, meaning you don’t get a period every 25-35 days. If your periods are every 40 or 45 days or further apart than that, don’t just think that that’s a good thing and that you’re saved from the pains of periods. That’s not normal and it does warrant an evaluation from an OBGYN.
At that appointment, they will test for reasons for irregular ovulation. There are other reasons that people don’t ovulate so they’re going to make sure there aren’t other things going on. If they think you have PCOS, they will screen you for some of the other medical conditions that I mentioned earlier and they will make sure that you are teed up. Then just follow up with some of those things at your annual checkup.
One of the mainstays of treatment for PCOS is regulating the menstrual cycle for those who are not trying to get pregnant. Usually, that’s done through hormonal treatment. Most commonly, the birth control pill, because the birth control pill can protect the uterus from uterine cancer. It can also treat some of the symptoms of PCOS, like irregular and sporadic bleeding. It can also treat and lower some of the testosterone and antigens that are high in patients who have PCOS, so it helps to improve their acne and decrease the amount of hair growth that they’re seeing. Typically some medications help regulate the cycle as recommended to help with some of the symptoms of PCOS.
TG: Can you share any insight into the seeming lack of research and information on this condition?
CC: There is a lot of research on PCOS and it’s something that’s been researched for over 25 years. I think the issue is that it is a very complex disease that involves your liver, it involves your ovaries, it involves your brain, it involves your uterus. It involves so many different things that I think pinpointing the reason is hard. There isn’t a way to reverse this hormonal imbalance.
I think a lot of patients come to me as a reproductive endocrinologist and say, “Hey Doc, can you balance my hormones?” Unfortunately, there isn’t something that can balance the hormones. This is the disease and we can treat the symptoms and be proactive about some of the lifestyle things that need to change in order to reduce the risk of some of the consequences. I wish there was a cure. It’s because it’s likely multifactorial [that] there isn’t one thing that can just make it all go away.
TG: What about PCOS is misunderstood?
CC: Not every patient with PCOS is going to be infertile. People [think], “Oh, because I have PCOS, I’m never going to have a baby; I’ll never get pregnant.” I do not want people to take that away from this conversation. There are many patients with PCOS who are able to get pregnant when they try. Don’t use PCOS as birth control because it’s not birth control—and you can definitely get pregnant with PCOS.
TG: Any final thoughts?
CC: If you are unsure if you’re ovulating, or don’t know when you’re ovulating, see a reproductive endocrinologist who can help you figure those things out and decide if treatment is necessary.

Kay Wicker is a lifestyle writer for theGrio covering health, wellness, travel, beauty, fashion, and the myriad ways Black people live and enjoy their lives. She has previously created content for magazines, newspapers, and digital brands.
TheGrio is FREE on your TV via Apple TV, Amazon Fire, Roku, and Android TV. TheGrio’s Black Podcast Network is free too. Download theGrio mobile apps today! Listen to ‘Writing Black’ with Maiysha Kai.