Editor’s note: The following article is an op-ed, and the views expressed are the author’s own. Read more opinions on theGrio.
In 2024, in the United States of America, it is still politically expedient to jeopardize the health of Americans who live and work in concentrated poverty and those without employer-sponsored health insurance. A high-stakes game is being played with health care access because, as a nation, we do not believe health care is a fundamental human and civil right. And because of this failure, the threat to the nation’s health is ever-present and growing.
Over 23 million Americans and counting have been disconnected from care. On April 1, 2023, when pandemic protections expired, states began to disenroll or terminate people from their Medicaid. This redetermination process had been halted temporarily during the public health emergency, but a little over a year ago, this harsh reality descended upon American families once again. Too often, Black and brown Americans, find themselves on the thorniest side of this equity disaster.
In a recent scorecard — researched and drafted by the NAACP and a coalition of civil rights and social justice partners — the performance rate of each state and the District of Columbia on Medicaid unwinding or disenrollments found that only one state received a passing grade. Only Hawaii voluntarily paused these terminations at the time of grade issuance. Rather, 25 states failed and another 25 states, including the District of Columbia, scored an incomplete. In life, an incomplete costs human lives and health, just like a failure.
So, as a nation, we are failing — again. And as egregious as it is, these losses are largely preventable.
As of June 14, 23,010,000 plus enrollees have been kicked off Medicaid across all 50 states and the District of Columbia. Though publicly available data is incomplete, best estimates place the burden of Medicaid unwinding on the backs of Black, Latino, Native/Indigenous, and Asian-American populations. It is projected that over half of those who have lost the benefit may be people of color based on known percentages of the program’s beneficiaries at baseline — historically, approximately 60% of Medicaid’s beneficiaries have been people of color. In another alarming statistic, over five million children have been dropped.The devastation across the lifespan is untenable. If we examine the net drop in enrollment in Medicaid, projected to be over 13 million, this is the arguably the worst decline in the program’s history.
Recommended Stories
A recent study published in JAMA examined those people, specifically, who lost their coverage due to procedural reasons from March 2023 through October 2023. This study is among the first comprehensive data sets to show how communities of color have been harmed by Medicaid disenrollments. According to researchers, Black and Latino/Hispanic Americans were two times as likely as their white peers to lose Medicaid last year because they were unable to complete the renewal application. Asian Americans were 1.5 times more likely to be impacted.
Across all states with available data, the Kaiser Family Foundation reports that 69% of those who were terminated lost their Medicaid due to procedural reasons. Meaning that an overwhelming majority of those who have been kicked off their health insurance happened because they did not complete the renewal process. This may happen when a state has outdated contact information, the enrollee doesn’t understand how to complete the application, or they miss the deadline. Therefore,many people who lost their Medicaid may indeed still be eligible by program criteria which makes the sting even more brutal. Administrative hurdles and red tape have ensnarled families already living in poverty, including children, and have left people saddled with chronic disease without critical access to care.
While some states have been forced to pause disenrollments to grapple with the onerous burden of procedural terminations, the performance across states has been uneven. While over 50 million people have had their Medicaid coverage renewed, recent polling shows that nearly 1 in 4 adults dumped from Medicaid are now uninsured. As many as 7 in 10 adults became uninsured during the unwinding process, at least temporarily. These numbers are more than stats, but represent families and people in our neighborhoods and social circles who have been pushed even closer to the Cliff of Good Health and sadly, some fell off. The survey also showed that almost 1 in 3 disenrolled adults found out at the point of care—either seeing a doctor or visiting the pharmacy — they had lost their Medicaid coverage.
Without health coverage, people face serious health and financial vulnerabilities. The human cost of being uninsured wreaks havoc on every aspect of life and only exacerbates pervasive health and health care disparities found in every state in this nation. According to the recent Commonwealth Fund report, stubborn racial and ethnic disparities persist throughout the health ecosystem: Black, Latino, and Indigenous communities experience higher rates of uninsurance, are more likely to forego medical care due to costs, and are more likely to be burdened with medical debt. Not to mention the unfair and unjust life tax that the burdens of racism, poverty, and resource/opportunity deprivation levy.
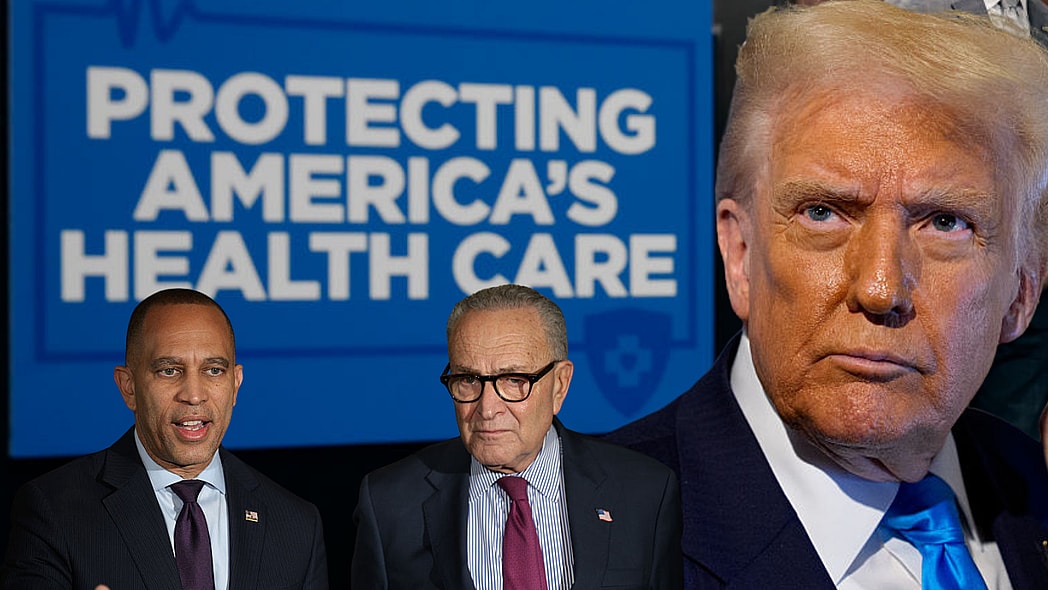
So, when we say, “Hands Off Our Health Care!” this is more than a slogan but a rallying cry for health and racial justice. To that end, the pursuit of health equity and the assurance of the conditions for optimal health for all people continues. And the demand in this next phase in our offensive is for governors and their state Medicaid directors to not only pause disenrollments, but to find ways efficiently and expediently to make the redetermination process more straightforward and automatic.
- As a priority, anyone who has been dropped from Medicaid and is deemed eligible should be re-enrolled;
- An automated renewal process that prevents procedural terminations should be established; and
- A paperless health care system based on Supplemental Nutrition Assistance Program (SNAP) records or tax returns should be implemented.
What the pandemic taught us, is that where there is political and human will, systems conspire to do courageous things. And when there is not, a survival of the fittest mentality picks off the most vulnerable, historically marginalized, and most overburdened communities. We refuse to unsee or unlearn these lessons. While there is a considerable burden for states to fix this policy nightmare which is costing the health and wellbeing of millions, given the sheer scope and disproportionate impact on historically marginalized groups, it is high time for the federal government to step in and commit to the assurance of a less onerous Medicaid system. Scapegoating on the backs of those who live in poverty or lack health coverage through their jobs is cruel and unusual punishment.
We can and must do better!
Derrick Johnson serves as president and CEO of the NAACP, a title he has held since October of 2017. President Johnson formerly served as vice chairman of the NAACP National Board of Directors, as well as state president for the Mississippi State Conference NAACP.
Dr. Chris T. Pernell is a dynamic physician leader and social change agent, serving as the Director of the NAACP Center for Health Equity. In her practice, she focuses on health justice, community-based advocacy, and population-wide health promotion and disease prevention.