In April, Grammy-winning singer and former “American Idol” contestant Mandisa was found dead in her home by friends. At just 47 years old, the star’s death was listed as “natural” in an autopsy report, which also determined that her death was a result of “complications of class III obesity.”
What is class III obesity?
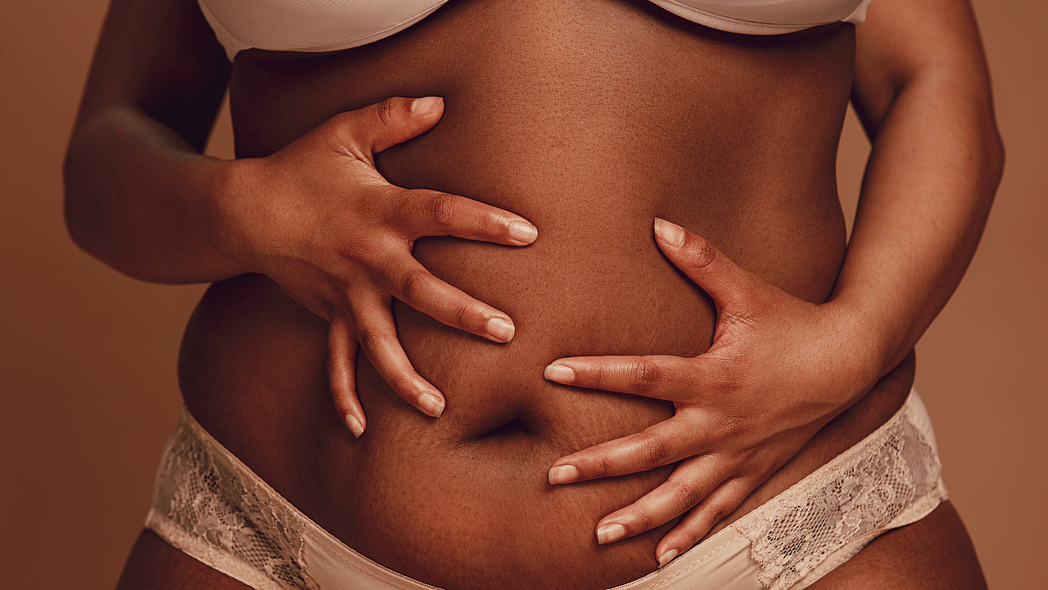
Scientifically, obesity is determined by an individual’s body mass index (BMI), which screens the amount of fat stored in the body using the ratio of an individual’s height and weight. According to the National Institutes of Health, class III obesity, formerly known as morbid obesity, refers to a BMI of 40 or higher. While BMI analytics are not always accurate for certain patients (like children), doctors use other tests to determine if a person is experiencing severe obesity. Other criteria for a class III diagnosis include being 100 pounds over the optimum body weight for a person’s gender and height, and/or having a BMI of 35 or more, and experiencing obesity-related health concerns like diabetes and high blood pressure.
Like the NIH, Dr. Nisha Parikh, assistant director for women’s heart health at Northwell, explained how this condition can significantly increase an individual’s risk of chronic disease and reduce overall health and quality of life.
“Obesity is definitely associated with premature deaths,” Parikh said, per People magazine. “[However it’s] probably not the obesity itself directly causing death in most cases, but rather the different conditions that obesity is associated with such as high blood pressure, diabetes, alterations in cholesterol, dyslipidemia (high cholesterol); obesity also predisposes to heart attacks, strokes, heart failure and even arrhythmias.”
Recommended Stories
Why it’s more than just “losing weight”
Throughout her career, Mandisa had been very candid about her weight loss journey, often pouring her feelings on the matter into her music while also celebrating and reflecting on the ups and downs of her journey.
“Beyond healthy eating and exercise is the mental and emotional health,” Mandisa told Essence magazine in 2020 after losing 80 pounds. “I’m a food addict, and just like an alcoholic, I tend to bury my troubles in something else. So even if I had lost the weight years ago, which I did, it would always come back until I learned to deal with my issues … I feel like I’ve done the gaining and losing so much that I can’t afford to go back to living that way.”
As Mandisa noted, obesity and weight can impact not only physical health but also mental health. In fact, the American Medical Association (AMA) recognizes obesity as a disease that involves genetic, metabolic, and behavioral symptoms that require mental assistance.
What can Black people learn from Mandisa’s obesity-related passing?
It is no secret that most times, Black people in the United States are more susceptible to a number of health concerns. Whether it’s a result of genealogy, lack of access to healthcare or discriminatory healthcare practices, Black communities face higher risks of diseases like obesity, diabetes, high blood pressure, heart disease, maternal mortality and more.
With over 108 million American adults currently living with obesity, unfortunately, 49.9% of non-Hispanic Black men fall under the category. Similarly, the U.S. Department of Health and Human Services’ Office of Minority Health found Black women have the highest rates of obesity or being overweight compared to other groups in the United States, with 4 out of 5 Black women considered overweight or obese.
“I believe that addressing the obesity epidemic in the Black community has never been more urgent,” Dr. Virginia A. Caine, a physician and the incoming president of the National Medical Association (NMA), wrote for theGrio. “…if we don’t take swift action to address and uplift the health of Black Americans — including ensuring access to critical, lifesaving medical treatments — we’ll lose an opportunity to reverse the consequences of obesity for millions of Black Americans. And those consequences are catastrophic.”
Living in an obesogenic society where Black Americans’ challenges with obesity are compounded by systemic struggles, it is important that those with access to medical care consult their doctors for support.
“See your doctor, first and foremost. Women in particular, our studies have shown, tend to go to the doctor less when we are overweight, or certainly even obese,” Parikh stressed, explaining how women often think they need to lose weight before seeing a physician. “I would counsel women to just stop that kind of thinking because, as physicians, we want to see you right now.”
Understanding the complex ways in which weight is discussed within the Black community, advocates and experts previously shared some simple actions Black Americans can take to get ahead of their obesity care. Revisit theGrio’s earlier reporting for these expert tips.